Forget CRP. Think Tregs
Low-Dose IL-2 Reduces Arterial Inflammation in ACS—Without Touching CRP
For decades, cardiology operated under a seductively simple premise: lower LDL, reduce events. Statins revolutionized secondary prevention. PCSK9 inhibitors pushed LDL into territories previously unimaginable. Yet patients kept dying.
This is the inconvenient truth of residual cardiovascular risk—the persistent hazard that remains despite optimal lipid-lowering therapy. In CANTOS, even with well-controlled LDL cholesterol, cumulative major cardiovascular event rates exceeded 20% at five years.
One in five patients. On guideline-directed therapy.
The culprit? Inflammation. The therapeutic response? Target IL-1β, measure CRP, declare victory when hsCRP drops. That was the playbook from CANTOS through COLCOT.
The CRP-Centric Era: What It Got Right and Wrong
The intellectual groundwork spans decades. Russell Ross’s “response to injury” hypothesis. Peter Libby’s meticulous characterization of inflammatory cell infiltration in atherosclerotic lesions. Paul Ridker’s epidemiological observations linking high-sensitivity C-reactive protein to cardiovascular events independent of LDL.
CANTOS delivered the proof. Canakinumab—a monoclonal antibody targeting interleukin-1β—reduced major adverse cardiovascular events by 15% in post-MI patients with hsCRP ≥2 mg/L. No change in lipids. The inflammatory hypothesis was validated.
The CRP responder analysis in CANTOS was striking: patients achieving on-treatment hsCRP <2 mg/L had a 25% reduction in MACE. Non-responders: 5%. CRP became both biomarker and therapeutic target.
But this created a blind spot. The field conflated inflammation reduction with CRP reduction. If hsCRP didn’t drop, was the intervention working?
IVORY answers: yes.
IVORY: Efficacy Without CRP Movement
The IVORY trial, published this month in Nature Medicine, takes a fundamentally different approach. Rather than blunting the IL-1β/IL-6/CRP axis, investigators amplified regulatory T cells—the adaptive immune system’s endogenous peacekeepers.
Low-dose interleukin-2 selectively expands Treg populations. At high doses, IL-2 activates cytotoxic T cells—hence its use in metastatic melanoma. But Tregs are enriched for the high-affinity trimeric IL-2 receptor (CD25/IL-2Rα), making them exquisitely sensitive to low concentrations. This pharmacological window enables precision immunomodulation.
The trial enrolled 60 ACS patients with hsCRP >2 mg/L, randomized to low-dose IL-2 (1.5 × 10⁶ IU) or placebo for 8 weeks. Arterial inflammation was quantified by ¹⁸F-FDG PET-CT.
Here’s what happened:
Arterial inflammation dropped 7.7% versus placebo (p=0.015).
In actively inflamed segments: 8.3% reduction (p=0.009).
In the most diseased segments: 9.3% reduction (p=0.010).
And hsCRP?
No difference between groups.
This is the paradigm shift: low-dose IL-2 reduced arterial inflammation through a CRP-independent mechanism. The inflammasome pathway and Treg-mediated immunoregulation are orthogonal.
The Immunological Mechanism: Tregs Reshape the Inflammatory Milieu
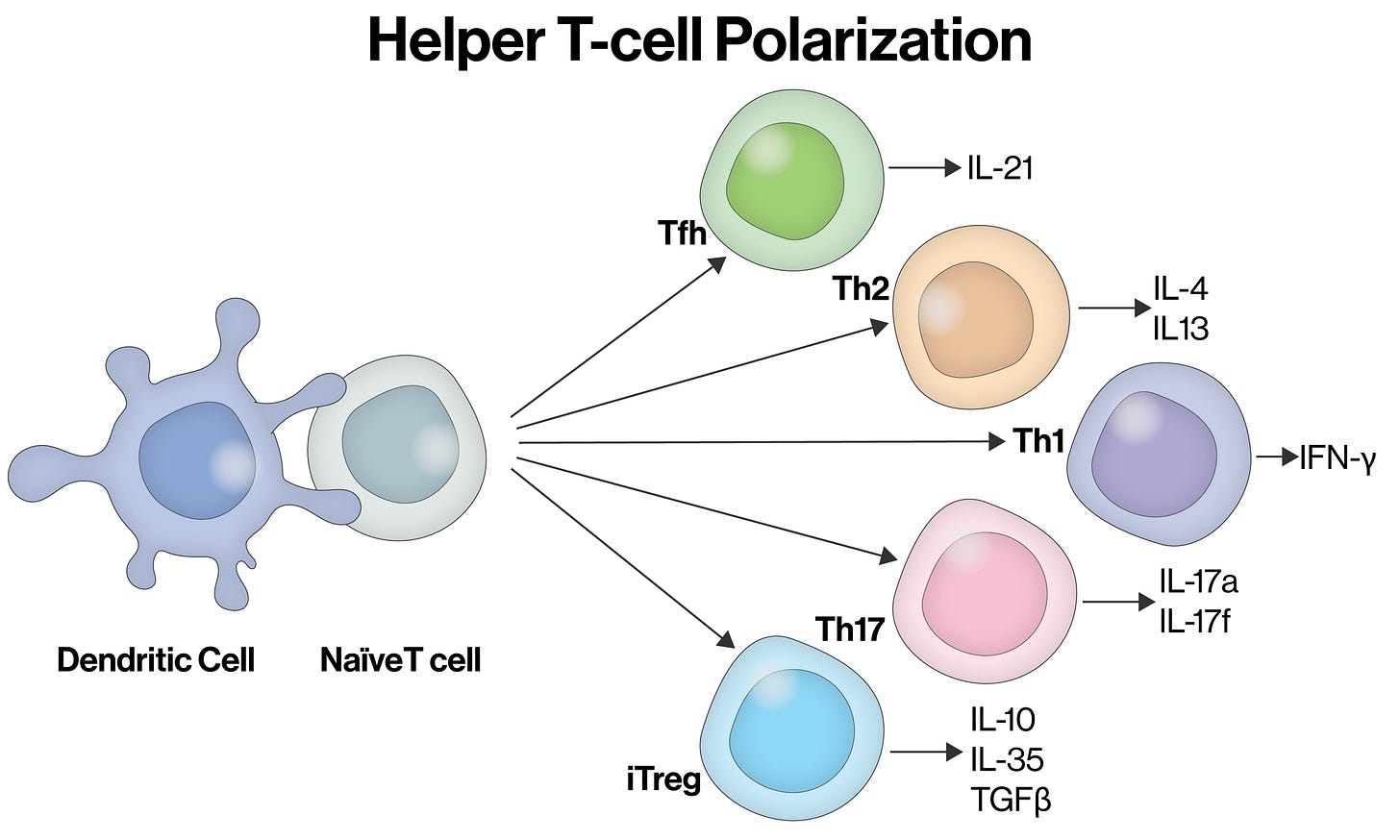
Regulatory T cells exert immunosuppression through multiple pathways: direct cell-cell contact via CTLA-4 and LAG-3, IL-2 consumption that starves effector T cells, secretion of IL-10 and TGF-β, and promotion of tolerogenic dendritic cell phenotypes.
In ACS patients, Tregs are depleted and dysfunctional. Mor and colleagues demonstrated reduced CD4+CD25+ Treg numbers in acute coronary syndromes back in 2006. Flego’s group later showed impaired CREB activation blocks Treg differentiation in NSTEMI patients.
IVORY reversed this deficit.
Treg cells increased 57% after the induction phase. During maintenance dosing, levels remained 34% above placebo. The adaptive immune system was reset.
But the immunological story extends beyond Treg expansion:
TH1 cells decreased — these IFN-γ producers drive plaque inflammation
T follicular helper cells decreased — reducing germinal center B cell activation
CD8+ cytotoxic T cells decreased — the effector arm was suppressed
The net effect: a comprehensive shift from pro-atherogenic to regulatory immune phenotype.
Importantly, in preclinical models, Treg expansion doesn’t just reduce inflammation—it promotes plaque stability. Meng et al. showed Tregs prevent plaque disruption in ApoE-knockout mice. Weirather’s group demonstrated Tregs improve post-MI healing by modulating monocyte/macrophage differentiation.
Regulation. Not suppression.
Effect Size in Context: Matching Statins without Touching Lipids
How meaningful is a 7-9% reduction in arterial inflammation?
High-intensity statins reduce arterial inflammation by ~10% versus low-intensity therapy. PCSK9 inhibition with alirocumab: ~8%. Low-dose IL-2 achieved comparable anti-inflammatory efficacy—on top of optimal medical therapy including high-dose statins in 98% of participants.
This is the key point. IVORY didn’t replace standard of care. It added orthogonal benefit. The anti-inflammatory effect was independent of lipid lowering, independent of CRP reduction, and additive to statins.
The dose-response relationship was also instructive: higher baseline inflammation predicted greater treatment effect. The sickest patients benefited most.
Safety: Why Immunomodulation Beats Immunosuppression
Anti-inflammatory therapy walks a tightrope. CANTOS demonstrated that potent IL-1β inhibition increases fatal infections. Colchicine carries gastrointestinal toxicity that limits adherence. And the recent CLEAR trial showed colchicine was ineffective in acute MI altogether.
Low-dose IL-2 threaded the needle.
Infection rates: 9% IL-2 versus 13% placebo. No difference.
The only significant adverse effect: injection site reactions in 91% of IL-2 recipients—mild, transient, resolved within 48 hours.
The cumulative IL-2 dose in IVORY was ~1.3% of oncology dosing. Treg expansion preserves host defense while attenuating pathological inflammation. This is pharmacological precision.
The 2-year follow-up from IVORY-FINALE strengthens the signal:
Zero MACE in the IL-2 arm.
Three patients in placebo experienced major adverse cardiovascular events.
Small numbers. Unambiguous direction.
Drug Development: The Adaptive Immunity Frontier Opens
The innate immune system—IL-1β, IL-6, NLRP3 inflammasome—has dominated cardiovascular drug development. CANTOS targeted IL-1β. Ziltivekimab targets IL-6 (ZEUS-CV ongoing). Colchicine acts through multiple innate pathways.
IVORY cracks open the adaptive immunity door.
Several development paths emerge:
Optimized IL-2 formulations. Engineering IL-2 muteins with enhanced Treg selectivity could improve the therapeutic index. Neoleukin-2/15 and similar next-generation constructs are in early development.
Combination strategies. Low-dose IL-2 did not reduce hsCRP, suggesting orthogonal mechanisms to IL-6 pathway inhibition. Combining Treg expansion with ziltivekimab could provide synergistic benefit—hitting both innate and adaptive arms.
Oral Treg-expanding agents. Injectable biologics face adherence challenges. Small molecules that selectively activate Treg-specific pathways represent the holy grail.
Antigen-specific tolerization. If atherosclerosis-associated autoantigens (oxidized LDL, ApoB100 peptides, heat shock proteins) can be definitively identified, tolerogenic vaccines could induce plaque-specific Tregs. Early preclinical work from Nilsson, Mallat, and others suggests feasibility.
The Bottom Line
CRP told us inflammation mattered.
Tregs show us how to control it.
IVORY demonstrates that harnessing adaptive immunity—specifically CD4+CD25+FoxP3+ regulatory T cells—safely reduces arterial inflammation in the highest-risk ACS patients. The mechanism is CRP-independent. The effect size matches statins. The safety profile outperforms canakinumab and colchicine.
This is not about replacing lipid management. Residual risk is multifactorial. But for ACS patients who remain inflamed despite guideline-directed therapy, the Treg pathway offers a genuinely new therapeutic axis.
The paradigm is shifting.
Forget CRP. Think Tregs.
The IVORY trial (NCT04241601) was published in Nature Medicine on January 8, 2026. The IVORY-FINALE study (NCT06427694) continues follow-up for cardiovascular outcomes through 5 years.


